How To Create A Psychiatric Tapering Crisis Plan

Creating a psychiatric tapering crisis plan is essential for managing the complexities of medication reduction. It requires a careful assessment of risks, clear guidelines for emergency responses, and ongoing support from trusted individuals.
By understanding how to monitor symptoms and adjust the tapering schedule with healthcare providers, you can better navigate potential crises. This structured approach not only promotes safety but also empowers you to make informed decisions during challenging times.
Key Takeaways
- Establish emergency response protocols that specify symptom thresholds for when to seek immediate medical intervention.
- Document clear roles for trusted individuals during crises and outline their responsibilities in support.
- Create a medication management plan with contingencies for returning to previous dosages if necessary.
- Implement daily symptom tracking to differentiate between withdrawal and relapse, along with regular check-ins with healthcare providers.
- Collaborate with healthcare teams to develop a tapering schedule tailored to medication type, dosage, and individual sensitivity.
Understanding Tapering Risks and Consequences
Understanding tapering risks and consequences is essential, especially as you navigate the potential complexities of reducing medications such as opioids or antidepressants.
Recognizing the risks of tapering is crucial when reducing opioid or antidepressant medications.
Tapering opioids can lead to a 57% increase in overdose or withdrawal incidents and a 52% rise in mental health crises within 12 to 24 months post-taper.
These elevated risks persist for up to two years after taper initiation.
Additionally, risks of overdose are particularly pronounced in patients with higher baseline opioid doses. Tapering antidepressants can result in withdrawal symptoms that may last weeks, months, or even years. Individual responses to tapering vary greatly, influenced by medication type, dosage and how long you have been taking them.
Meticulous monitoring and tailored tapering strategies are vital to mitigate adverse effects and support your mental health during this challenging process.
Prioritize your safety and well-being throughout the tapering journey.
Essential Crisis Plan Components
Developing an effective crisis plan is essential for anyone undergoing tapering, as it provides a structured approach to manage potential mental health emergencies.
A thorough plan includes emergency response protocols that identify specific symptom thresholds necessitating immediate medical intervention, such as suicidality or severe withdrawal. You should differentiate between symptoms requiring an emergency department visit versus outpatient care.
Integrating a support system is crucial; designate trusted individuals with clearly defined roles during crises. Document medication management contingencies, including predefined parameters for returning to previous dosages and access to "rescue medications."
Finally, advance care directives outlining treatment preferences during incapacitating episodes should be prepared, ensuring emergency personnel can access these documents quickly. This approach emphasizes the importance of integrated support during the tapering process to enhance overall recovery and resilience.
Monitoring and Early Warning Signs
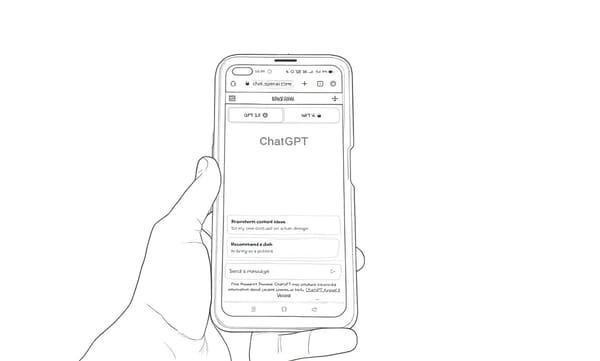
As you navigate the tapering process, monitoring your symptoms and recognizing early warning signs becomes essential for maintaining mental health stability. Keeping a close watch on your symptoms helps differentiate between withdrawal and relapse, which may manifest at different times.
Utilize daily symptom tracking, and check in weekly with your healthcare provider to assess your physical and psychological state. It’s important to remember that tapering should be done under provider supervision, as this can help ensure a safe and effective process.
Response Protocols for Crisis Situations
Crisis situations can arise unexpectedly, necessitating well-defined response protocols to guarantee effective intervention and support. Standardized risk evaluation tools are essential for determining suicide risk and potential harm to others, differentiating low, medium, and high-risk scenarios.
Immediate access to crisis support is available through 24/7 call centers and mobile crisis teams, ensuring timely intervention. It's vital to have clear criteria for measuring imminent risk, focusing on suicidal intent, plan credibility, and access to means.
For low-risk individuals, follow-up should occur within two weeks, while medium-risk cases require a one-week follow-up. High-risk situations trigger immediate team notifications and potential emergency services activation. These protocols prioritize safety and appropriate intervention to effectively manage crises.
Having a crisis plan ensures patient safety beyond available hours, providing essential resources during distress.
Collaborative Planning With Healthcare Providers
Effective collaboration with healthcare providers is vital for creating a tapering plan that accommodates individual patient needs and promotes safety.
Primary care providers play an important role, often prescribing medications for anxiety or depression and delivering long-term mental health care. Regular communication with your healthcare team guarantees that discussions about tapering include timeline expectations, monitoring frequency, and backup plans.
The design of tapering schedules should consider medication type, current dosage, and individual sensitivity. Thorough assessments of your history, potential withdrawal symptoms, and stress levels guide the development of a tailored tapering plan.
Primary care providers are expected to manage complex mental health tasks, making their involvement crucial in this process.
Engaging in collaborative care programs can enhance support, connecting you with care managers and specialists who guarantee a safe and effective tapering process.
Tapering Schedule Adjustments During Crisis
Collaborative planning with healthcare providers lays the groundwork for effective tapering strategies, but unexpected crises can considerably impact these plans.
During a crisis, it’s essential to adjust your tapering schedule to guarantee safety and well-being. Here are three key modifications to take into account:
- Smaller Dose Reductions: If severe withdrawal symptoms emerge, reduce your doses more gradually to minimize discomfort. Gradual tapering is crucial to avoid exacerbating withdrawal effects.
- Extended Time Frames: Allow more time between dose reductions, confirming symptoms have subsided before proceeding.
- Immediate Responses: If relapse symptoms occur, return to your previous stable dosage before attempting to taper again.
These adjustments help manage the risks associated with tapering and support a safer recovery process during difficult times.
Always prioritize communication with your healthcare provider throughout this journey.
Conclusion
Creating a psychiatric tapering crisis plan is essential for ensuring safety during medication adjustments.
As the saying goes, "An ounce of prevention is worth a pound of cure."
By understanding tapering risks, establishing a thorough crisis plan, and collaborating with healthcare providers, you can navigate potential challenges more effectively. Regularly monitoring symptoms and adjusting the tapering schedule as needed will also enhance your support system, ultimately fostering a healthier path toward recovery.